Epidural steroid injections have been used for many years in the treatment of spinal pain. One of the first references to epidural injection was made in 1920 in the treatment of low back pain and sciatica. Epidural corticosteroid injection is often used for diseases such as spinal stenosis, intradiscal degeneration, herniated intervertebral disc, sciatica and radiculopathy. Cervical and thoracic epidural injection is used also in the treatment of post-herpetic neuralgia. The technique is applied in the subacute phase of a painful condition (e.g. sciatica) and in the chronic phase of some diseases (e.g. spinal stenosis) when the pain does not subside with conservative treatment.
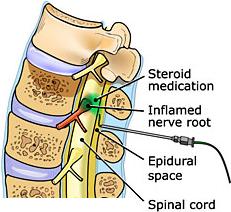
Corticosteroids injected in the region of inflamed nerve roots, have a strong anti-inflammatory action reducing the oedema and relieving pain. The solution injected contains also local anaesthetic, usually ropivacaine, which offers immediate relief lasting for some hours. The corticosteroid (usually depot-medrol, betamethasone or dexamethasone) will start acting 3-5 days after the injection and the result lasts from some weeks to some months. The technique may need to be repeated up to two more times, with an inbetween interval of at least 2 weeks. In general, no more than 3 injections should be done within a period of 6 months. Should the pain not subside, other therapies have to be found.
Epidural corticosteroid injection does not treat the actual cause of the disease (e.g. the herniated intervertebral disc). It rather gives time to nature itself to regress the disc herniation by offering analgesia reducing the inflammation of the nerve root that causes the pain. Besides, think of how many people show herniated intervertebral discs in their MRI but have no actual disturbance at all!
 ANATOMY RELEVANT TO THE TECHNIQUE
ANATOMY RELEVANT TO THE TECHNIQUE
The spinal cord, located within the spinal canal, is surrounded by three layers of protective membranes that are called meninges. The three meninges, starting from the innermost to the outermost, are the following: pia, arachnoid and dura mater.
Inbetween the three meninges there is anatomical space of very small dimensions, Between the pia and arachnoid mater there is the subarachnoid space, within which circulates the cerebrospinal fluid (CSF). Between the arachnoid and dura mater, there is a tiny space, the subdural space. Above the dura mater and between itself and ligamentum flavum, there is the epidural space containing fat and the nerve roots exiting from the spinal cord.
The epidural space extends along the spine, from the occipital foramen to approximately the 2nd sacral level. These nerve roots going through the epidural space and leaving the spine through the intervertebral foramina, constitute the target of the epidural injection.
There are three different techniques for applying this therapeutic method, known as translaminar, transforaminal and sacrococcygeal epidural injection. The selection of the technique depends on the disorder in question and the particularity of each patient. There is no need for hospitalization and the patient can go home very soon after the application. The technique is performed under local anaesthesia, with the patient in the prone position and a pillow placed under the abdomen. A special needled is advanced to the target point under fluoroscopic guidance and then contrast medium is infused to confirm the proper positioning of the needle tip. As long as the therapist physician is satisfied with the needle position, the corticosteroid-local anaesthetic solution is injected and the needle is removed. The needle site is covered with antiseptic and gauze.
• Translaminar approach. The needle is inserted from the posterior surface of the vertebral body and is directed between the spinous processes of the spine. Spinous processes are the bones that protrude when bending forwards. The drug solution that is injected “washes” the nerve roots in both sides of the spine at the level of injection. (4,5,6,16)
• Transforaminal approach. The needle is placed exactly into the intervertebral foramen from where the nerve root exits the spine. It is the ideal technique for applying an anti-inflammatory therapy, in an absolutely selective way, to some inflammed nerve root that causes pain (e.g. sciatica due to subacute herniated intervertebral disc). Ackerman and Ahmad (2007) proved that the transforaminal approach is more effective than translaminar and sacrococcygeal approaches in the treatment of herniated intervertebral disc and radicular pain at the level between the 5th lumbar and 1st sacral spine. (11,12,18)
• Sacrococcygeal approach. Sacrum is the last level of the spine that connects the spine with the hips. The needle is inserted into the epidural space through a small opening in the sacrum called sacral hiatus. The technique is applied for the treatment of low back pain and sciatica. (1,2,13)
RISKS -COMPLICATIONS
Epidural corticosteroid injection is a relatively safe technique with a very low rate of complications. Complications that have been reported are epidural haematoma, abscess, Cushing syndrome, anaphylactoid reaction and headache in case there is injury of the dura mater and loss of cerebrospinal fluid (CSF).
CONTRAINDICATIONS
Epidural injection should not be applied when the patient has any blood coagulation disorder or receives anticoagulants. In the latter case, the regimen should be discontinued for quite a sufficient time and the oral anticoagulant should be replaced with low molecular weight heparin, always with the therapist physician’s approval.
RESULTS
The degree and duration of pain relief following a therapeutic epidural injection, differ from case to case and depend on many other factors, such as the patient’s medical history and activity level. Some patients may be permanently relieved with one or two injections, whereas others may be relieved only temporarily.
The Physical Medicine and Rehabilitation Department of Washington University have carried out a study comparing outcome and risks between surgical treatment and epidural corticosteroid injection.
It has been concluded from the study that lumbar epidural corticosteroid injection is a treatment that should precede the surgical lumbar spine operation, unless the patient’s highly severe neurological symptomatology strictly requires immediate surgery.
LITERATURE
1. Viner N. Intractable sciatica: the sacral epidural injection—an effective method of giving relief. Can Med Assoc J. 1925;15:630–634.
2. Evans W. Intrasacral epidural injections in the treatment of sciatica. Lancet. 1930;219:1225–1229.
3. Brown JH. Pressure caudal anaesthesia and back manipulation. Northwest Med (Seattle). 1960;59:905–909.
4. Goebert HW, Jallo SJ, Gardner WJ, Wasmuth CE, and Bitte EM. Sciatica: treatment with epidural injections of procaine and hydrocortisone. Cleveland Clinic Quart. 1960;27:191–197.
5. Williams KD, Park AL. Lower back pain and disorders of intervertebral discs. In: Canale ST, Beaty JH, eds. Campbell’s Operative Orthopedics. 11th ed. Philadelphia, PA: Mosby Elsevier; 2008: 2159-2223.
6. Levin KH. Nonsurgical interventions for spine pain. Neurological clinics. 2007;25(2):495-505.
7. Heran MKS, Smith AD, Legiehn GM. Spinal injection procedures: a review of concepts, controversies, and complications. Radiol Clin of North Am. 2008;46(3):487-514.
8. Ackerman WE 3rd, Ahmad M. The efficacy of lumbar epidural steroid injections in patients with lumbar disc herniations. Anesth Analg. 2007;104(5):1217-22.
9. Papagelopoulos PJ, Petrou HG, Triantafyllidis PG, et al. Treatment of lumbosacral radicular pain with epidural steroid injections. Orthopedics. 2001;24(2):145-149.
10. McLain RF, Kapural L, Mekhail NA. Epidural steroid therapy for back and leg pain: mechanisms of action and efficacy. Spine J. 2005;5(2):191-201.
11. Botwin KP, Gruber RD, Bouchlas CG, et al. Fluoroscopically guided lumbar transformational epidural steroid injections in degenerative lumbar stenosis: an outcome study. Am J Phys Med Rehabil. Dec 2002;81(12):898-905.
12. Buenaventura RM, Datta S, Abdi S, et al. Systematic review of therapeutic lumbar transforaminal epidural steroid injections. Pain Physician. 2009;12(1):233-51.
13. Sayegh FE, Kenanidis EI, Papavasiliou KA, Potoupnis ME, Kirkos JM, Kapetanos GA. Efficacy of steroid and nonsteroid caudal epidural injections for low back pain and sciatica: a prospective, randomized, double-blind clinical trial. Spine. 2009;34(14):1441-1447.
14. Conn A, Buenaventura RM, Datta S, et al. Systematic review of caudal epidural injections in the management of chronic low back pain. Pain Physician. 2009;12(1):109-35.
15. Abdi S, Datta S, Trescot AM, Schultz DM, Adlaka R, Atluri SL, Smith HS, Manchikanti L. Epidural steroid in the management of chronic spinal pain: a systematic review. Pain Physician. 2007;10(1):185-212.
16. Parr AT, Diwan S, Abdi S. Lumbar interlaminar epidural injections in managing chronic low back and lower extremity pain: a systematic review. Pain Physician. 2009;12(1):163-88.
17. Rydevik BL, Cohen DB, Kostuik JP: Spine epidural steroids for patients with lumbar spinal stenosis. Spine. 1997;22:2313-2317.
18. Huntoon MA, Martin DP: Paralysis after transforaminal epidural injection and previous spinal surgery. Reg Anesth Pain Med. 2004;29:494-495.19. Botwin KP, Gruber RD, Bouchlas CG, et al: Complications of fluoroscopically guided transforaminal lumbar epidural injections. Arch Phys Med Rehabil 2000; 81:1045-1050.