GENERAL
The sacroiliac joint is a quite common cause of chronic low back pain. According to the criteria set by the International Association for the Study of Pain (IASP), the sacroiliac joint pain is defined as the pain which is located in the sacroiliac joint, reproduced with provocation and stress-inducing tests of the joint and significantly relieved with selective injection of local anaesthetic into the sacroiliac joint. (3)
Patients suffering from pain of the sacroiliac joint find difficulty in carrying out daily activities, such as walking, sitting, standing up and even sleeping. The reported incidence of sacroiliac joint pain in patients with chronic low back pain ranges between 16% and 30%. (4-6) However, there are many people suffering for months -or even years- until the proper diagnosis is set. Quite often the pain is wrongly attributed to the hip joints or to a nerve root inflammation, due to a herniated intervertebral disc that was revealed by MRI.
 ANATOMY OF THE SACROILIAC JOINT
ANATOMY OF THE SACROILIAC JOINT
Sacroiliac joints transfer the body weight towards the lower limbs. Thus, they are joints carrying high loads of weight. They are located in the buttocks region and are covered with quite many groups of muscles and ligaments. There are two sacroiliac joints -one at each side of the pelvis- connecting the iliac bones with the sacrum. Iliac bones are the bones that form the pelvis. The sacrum is composed of fused vertebrae below the 5th lumbar vertebra (L5). The sacroiliac joints have very strong ligaments and cartillage to absorb vibrations and allow some mobility to the joint.
CAUSES OF PAIN
The sacroiliac joint pain can be either of intra-articular aetiology (infection, arthritis, spondyloarthropathy, malignancy) or of extra-articular aetiology (fractures, injury of ligaments and myofascia). Very often the pain is present but no specific cause can be identified. Poor support, repetitive rotational forces on the pelvis and inflammation may also induce pain.
Risk factors are lower-limb asymmetry, injuries, scoliosis, lumbar spine fusion, heavy physical activity and pregnancy. (8-13) It is characteristic that patients with chronic low back pain who have undergone a successful lumbar spine fusion, , may manifest sacroiliac joint pain (identified with diagnostic intra-articular block) in a rate between 32% and 35%. (11)
DIAGNOSIS
In general, the sacroiliac joint pain is located in the buttocks region (94%). Patients may report pain radiating to the lower lumbar spine (72%), groin region (14%), upper lumbar spine (6%) or abdomen (2%). Pain radiating to lower limbs down to knee height is reported in 28% of patients, whereas about 12% of patients report pain extending all the way down the feet. (17,18)
Various diagnostic tests are applied for the clinical evaluation of the sacroiliac joint aiming at stressing the suspicious joint and provoking pain to the patient. When at least three tests provoke pain, the odds for positive diagnosis increase significantly.
SUPPLEMENTARY EXAMINATIONS
Radiodiagnostic examinations are useful only for ruling out other serious conditions. They are not sufficient to give the diagnosis for there is no correlation between the MRI findings and the sacroiliac joint pain that has been identified with diagnostic block.
According to the IASP criteria, the sacroiliac joint pain should be eliminated immediately after a successful local anaesthetic injection in the joint. (5,7,14,23) Following the injection, the patient is able to make movements (with great ease) that s/he could not do before the block and reports impressive improvement in physical ability. The result of a positive diagnostic block for the sacroiliac joint pain is temporary and lasts for as long as the duration of the anaesthetic.
In order for the diagnostic block to be applied properly and for its result to be considered reliable, the technique has to be conducted under radiological guidance and without administrating any painkiller or sedative before or during the operation. (23) A study has demonstrated that only 22% of blind applications (i.e. without radiological guidance) have resulted in successful intra-articular sacroiliac injection. (28)
TREATMENT
A. CONSERVATIVE TREATMENT
The conservative treatment includes combination of rest, pharmacotherapy, ice therapy and physiotherapy.
The drugs administered are simple analgesics, such as paracetamol and anti-inflammatory drugs, which reduce inflammation and at the same time limit pain.
In case the conservative treatment fails and pain persists for a period longer than three months, there are minimally invasive techniques specially designed for the relief of sacroiliac joint pain.
1.  Intra-articular injection of corticosteroids and local anaesthetic. The injection can be repeated after 15-20 days, depending upon the result of the first injection. If the relief achieved has a long duration (e.g. 6 months), another dose can be repeated (in total, three doses per year). (26,27,32)
Intra-articular injection of corticosteroids and local anaesthetic. The injection can be repeated after 15-20 days, depending upon the result of the first injection. If the relief achieved has a long duration (e.g. 6 months), another dose can be repeated (in total, three doses per year). (26,27,32)
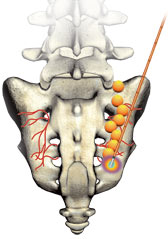 2. Radiofrequency sacroiliac joint denervation. This technique is applied in case the previous invasive therapeutic method has failed. The result of denervation is not guaranteed, because the sacroiliac joint innervation is very rich and the course of nerve branches is not that predictable. However, it is a minimally invasive therapeutic technique, with only a few reported complications, and it should be conducted when no other satisfactory pain treatment is found. (35,36,37,38,39)
2. Radiofrequency sacroiliac joint denervation. This technique is applied in case the previous invasive therapeutic method has failed. The result of denervation is not guaranteed, because the sacroiliac joint innervation is very rich and the course of nerve branches is not that predictable. However, it is a minimally invasive therapeutic technique, with only a few reported complications, and it should be conducted when no other satisfactory pain treatment is found. (35,36,37,38,39)
3. Neurostimulation with implantation of subcutaneous electrodes in the sacroiliac joint region. It is a method that is not scientifically evidence-based for the treatment of sacroiliac joint pain. Yet, there are some case reports in which the specific therapeutic technique was tried and the result has been satisfactory,. The advantage of this method is that electrodes are placed easily with local anaesthesia and about a one-week testing period follows with an external generator. So, if the patient reports a significant (over 50%) improvement of pain, a final implantation of the neurostimulation system is conducted subcutaneously.
MEDICAL INFORMATION SOURCES
1. PAIN PRACTICE JOURNAL
2. BONICA”S MANAGEMENT OF PAIN
3. PAIN PHYSICIAN JOURNAL
4. INTERVENTIONAL PAIN MANAGEMENT BOOK
5. NEUROMODULATION JOURNAL
Literature
1. Guyatt G, Gutterman D, Baumann MH, et al.
Grading strength of recommendations and quality of
evidence in clinical guidelines: report from an American
College of Chest Physicians Task Force. Chest. 2006;129:174–
181.
2. van Kleef M, Mekhail N, van Zundert J. Evidencebased
guidelines for interventional pain medicine according to
clinical diagnoses. Pain Pract. 2009;9:247–251.
3. Merskey H, Bogduk N. Classification of Chronic
Pain: Descriptions of Chronic Pain Syndromes and Definitions
of Pain Terms. 2nd ed. Seattle, WA: IASP Press; 1994.
4. Bernard TN Jr, Kirkaldy-Willis WH. Recognizing
specific characteristics of nonspecific low back pain. Clin
Orthop Relat Res. 1987;266–280.
5. Schwarzer AC, Aprill CN, Bogduk N. The sacroiliac
joint in chronic low back pain. Spine. 1995;20:31–37.
6. Maigne JY, Aivaliklis A, Pfefer F. Results of sacroiliac
joint double block and value of sacroiliac pain provocation
tests in 54 patients with low back pain. Spine.
1996;21:1889–1892.
7. Fortin JD, Kissling RO, O’Connor BL, Vilensky JA.
Sacroiliac joint innervation and pain. Am J Orthop.
1999;28:687–690.
8. Schuit D, McPoil TG, Mulesa P. Incidence of sacroiliac
joint malalignment in leg length discrepancies. J Am
Podiatr Med Assoc. 1989;79:380–383.
9. Herzog W, Conway PJ. Gait analysis of sacroiliac
joint patients. J Manipulative Physiol Ther. 1994;17:124–127.
10. Schoenberger M, Hellmich K. Sacroiliac dislocation
and scoliosis. Hippokrates. 1964;476–479.
11. Katz V, Schofferman J, Reynolds J. The sacroiliac
joint: a potential cause of pain after lumbar fusion to the
sacrum. J Spinal Disord Tech. 2003;16:96–99.
12. Marymont JV, Lynch MA, Henning CE. Exerciserelated
stress reaction of the sacroiliac joint. An unusual cause
of low back pain in athletes. Am J Sports Med. 1986;14:320–
323.
13. Albert H, Godskesen M, Westergaard J. Prognosis in
four syndromes of pregnancy-related pelvic pain. Acta Obstet
Gynecol Scand. 2001;80:505–510.
14. Slipman CW, Jackson HB, Lipetz JS, et al. Sacroiliac
joint pain referral zones. Arch Phys Med Rehabil. 2000;
81:334–338.
15. Laslett M, Aprill CN, McDonald B, Young SB.
Diagnosis of sacroiliac joint pain: validity of individual provocation
tests and composites of tests. Man Ther. 2005;10:207–
218.
16. van der Wurff P, Buijs EJ, Groen GJ. A multitest
regimen of pain provocation tests as an aid to reduce unnecessary
minimally invasive sacroiliac joint procedures. Arch
Phys Med Rehabil. 2006;87:10–14.
17. Szadek KM, van der Wurff P, van Tulder MW,
Zuurmond WW, Perez RS. Diagnostic validity of criteria for
sacroiliac joint pain: a systematic review. J Pain. 2009;10:354–
368.
18. Young S, Aprill C, Laslett M. Correlation of clinical
examination characteristics with three sources of chronic low
back pain. Spine J. 2003;3:460–465.
19. Bigos S, Bowyer O, Braen G, et al. Acute low back
pain problems in adults. Clinical Practice Guideline No. 14.
AHCPR Publication No. 95-0642. Rockville, MD: Agency for
Healthcare Policy and Research, Public Health Service, U.S.
Department of Health and Human Services; December 1994.
20. Hansen HC, McKenzie-Brown AM, Cohen SP, et al.
Sacroiliac joint interventions: a systematic review. Pain Physician.
2007;10:165–184.
21. Puhakka KB, Jurik AG, Schiottz-Christensen B, et al.
MRI abnormalities of sacroiliac joints in early spondylarthropathy:
a 1-year follow-up study. Scand J Rheumatol.
2004;33:332–338.
SIJ Pain • 477














