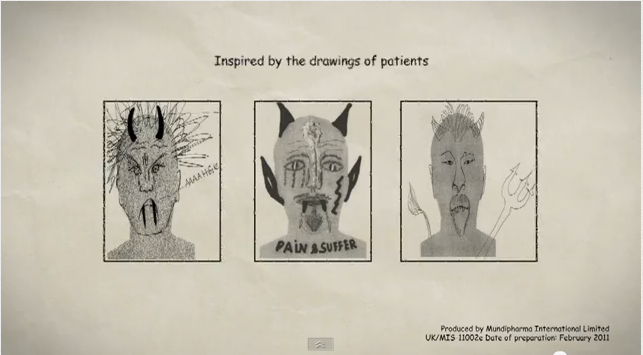
Magnetic resonance imaging (MRI) of the spine is a very useful test, which without the patient received radiation, gives us much information about the condition of vertebrae, intervertebral discs, nerve roots, the height of the intervertebral spaces and the zygoapophyseal joints. But still remains an image that describes morphological anatomical details of the spine, without this meaning that it can prove the cause of an acute or chronic pain of the spine with or without radiation to the extremities.
According to studies carried out in a large number of people, proved that a large percentage of people examined with an MRI at the lumbar region of the spine, showed severe morphological abnormalities in the anatomical structures , although the same people were totally asymptomatic.
MRI results in normal humans examined with MRI (number of patients= 67)
Cleveland Pain Clinic USA
| Under Age 60 | Over 60 |
|
| Herniated intervertebral disc | 22% | 36% |
| Spinal stenosis | 1% | 21% |
| Disc prolapse |
54% |
79% |
| Intervertebral disc degeneration | 46% | 93% |
We conclude therefore that the most important in identifying the cause of spinal pain is a good history, clinical examination of the patient and the findings correlated with laboratory findings, among them, and MRI.
So when a patient first goes to the doctor complaining of back pain or sciatica, should not undergo MRI, but can be treated conservatively or by minimally invasive techniques for at least 4-6 weeks. If pain persists, you may request additional examinations likemagnetic resonance imaging. The exception to this rule is the recognition by the physician during the first clinical examination, dangerous and serious neurological signs that require immediate surgery . In this case prior to surgery, examination of the spine with MRI is indicated
Is therefore clear that the physician should treat the patient, rather than MRI, which in some cases, unfortunately, is used to drive the patient to surgery and to undergo substance in an unnecessary surgery which not only cures the real cause of pain, but can often lead to disaster (-Boden et al., JBJS, 1990) and cause additional and more serious problems such as permanent chronic neuropathic pain after laminectomy, chronic sciatica from nerve entrapment by postoperative scar tissue, spinal instability, etc.