Compression fractures due to osteoporosis occur to quite a great number of people annually. The most frequent among them are hip fractures resulting in prolonged disability and severe pain.
Until recently, physicians had limited therapeutic options to treat spinal fractures. These included analgesics, rest and immobilization to bed, tight spine bandaging and surgical spine fusion. Today there are two minimally invasive techniques treating pain directly and stabilizing the spine. These are spondyloplasty and kyphoplasty.
It is a non-surgical intervention performed under fluoroscopic guidance, local anaesthesia and light sedation. The patient is placed in the prone position and, once the region is carefully sterilized, a special needle is advanced through the vertebral pedicle into the vertebral fractured body. The proper and safe advancement and final position of the needle are continuously controlled with fluoroscopic views in the anteroposterior and lateral position.
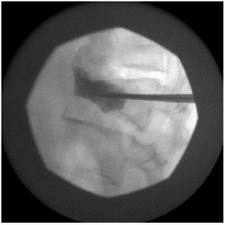 A small amount of acrylic cement is advanced into the vertebral body through the lumen of the needle. Acrylic cement is a type of medical cement used for many years in various orthopaedic surgical operations. When the cement is injected, it has the form of a toothpaste and, the minute it gets into the vertebra, it instantly sets. A few hours after the completion of spondylopasty, the patient is in the position to walk without pain and go home even on the very same day. (6,7,8,9)
A small amount of acrylic cement is advanced into the vertebral body through the lumen of the needle. Acrylic cement is a type of medical cement used for many years in various orthopaedic surgical operations. When the cement is injected, it has the form of a toothpaste and, the minute it gets into the vertebra, it instantly sets. A few hours after the completion of spondylopasty, the patient is in the position to walk without pain and go home even on the very same day. (6,7,8,9)
Kyphoplasty is a more recent technique for the treatment of compression vertebral fractures. It is applied under local anaesthesia and fluoroscopic guidance. Its advantage compared to spondyloplasty is that at the same time it relieves pain and also stabilizes the spine and restores its height and deformity. Also, the cement that needs to be injected is better controlled minimizing the chances to leak into the spinal canal. A working cannula is placed at the affected vertebral body through the pedicle bilateral to the spine. The bone is trephined and then a special balloon is placed at each side. These balloons are filled with contrast medium, controlled with a special device measuring pressure and monitored with fluoroscopy. When the desirable height and shape of the vertebral body has been achieved, the balloons are deflated and withdrawn. The cavity they have formed is immediately filled with acrylic cement which rapidly sets and stabilizes the vertebra in its proper position. Some hours later the patient is able to fully move without any pain. (6,11,12,13,14)
RISKS – COMPLICATIONS
The main danger is related to the positioning of the needle and injection of the cement. The cement may leak backwards and exert pressure on the nerve roots or spinal cord, causing permanent impairment. Although this is a serious and dangerous complication, it occurs extremely rarely in less than 1% of patients. According to a review of the American Food and Drug Association (FDA), for the period 1999-2003 there were 58 complications reported out of 200.000 applications of the technique. Other potential complications are haemorrhage, infection and persistent pain. (4,5)
LITERATURE
1. Stallmeyer MJB, Zoarski G: Patient evaluation and selection. In Percutaneous Vertebroplasty and Kyphoplasty, edn 2. Edited by Mathis JM, Deramond H, Belkoff SM. New York: Springer; 2006:60–61.
2. Huang C, Ross PD, Wasnich RD: Vertebral fracture and other predictors of physical impairment and health care utilization. Arch Intern Med 1996, 156:2469–2475.
3. Tosteson AN, Hammond CS: Quality-of-life assessment in osteoporosis: health-status and preference-based measures. Pharmacoeconomics 2002, 20:289–303.
4. Lindsay R, Silverman SL, Cooper C, et al.: Risk of new vertebral fracture in the year following a fracture. JAMA 2001, 285:320–323.
5. Charnley J: The reaction of bone to self-curing acrylic cement. A long-term histological study in man. J Bone Joint Surg Br 1970, 52:340–353.
6. Galibert P, Deramond H: Percutaneous acrylic vertebroplasty as a treatment of vertebral angioma as well as painful and debilitating diseases. Chirurgie 1990, 116:326–334; discussion 335.
7. Galibert P, Deramond H, Rosat P, et al.: Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty. Neurochirurgie 1987, 33:166–168.
8. Jensen ME, Evans AJ, Mathis JM, et al.: Percutaneous polymethylmethacrylate vertebroplasty in the treatment of osteoporotic vertebral body compression fractures: technical aspects. AJNR Am J Neuroradiol 1997, 18:1897–1904.
9. Kaemmerlen P, Thiesse P, Jonas P, et al.: Percutaneous injection of orthopedic cement in metastatic vertebral lesions. N Engl J Med 1989, 321:121.
10. Lieberman IH, Dudeney S, Reinhardt MK, et al.: Initial outcome and efficacy of “kyphoplasty” in the treatment of painful osteoporotic vertebral compression fractures. Spine 2001, 26:1631–1638.
11. McGraw JK, Cardella J, Barr JD, et al.: Society of Interventional Radiology quality improvement guidelines for percutaneous vertebroplasty. J Vasc Interv Radiol 2003, 14:827–831.
12. Liu JT, Liao WJ, Tan WC, et al.: Balloon kyphoplasty versus vertebroplasty for treatment of osteoporotic vertebral compression fracture: a prospective, comparative, and randomized clinical study. Osteoporos Int 2010 21:359-364
13. Garfin SR, Yuan HA, Reiley MA: New technologies in spine: kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures. Spine 2001, 26:1511–1515.
14. Nussbaum DA, Gailloud P, Murphy K: A review of complications associated with vertebroplasty and kyphoplasty as reported to the Food and Drug Administration medical device related web site. J Vasc Interv Radiol 2004, 15:1185–1192.















